Table of Contents
ToggleConcussion. What prognostic factors guide recovery?
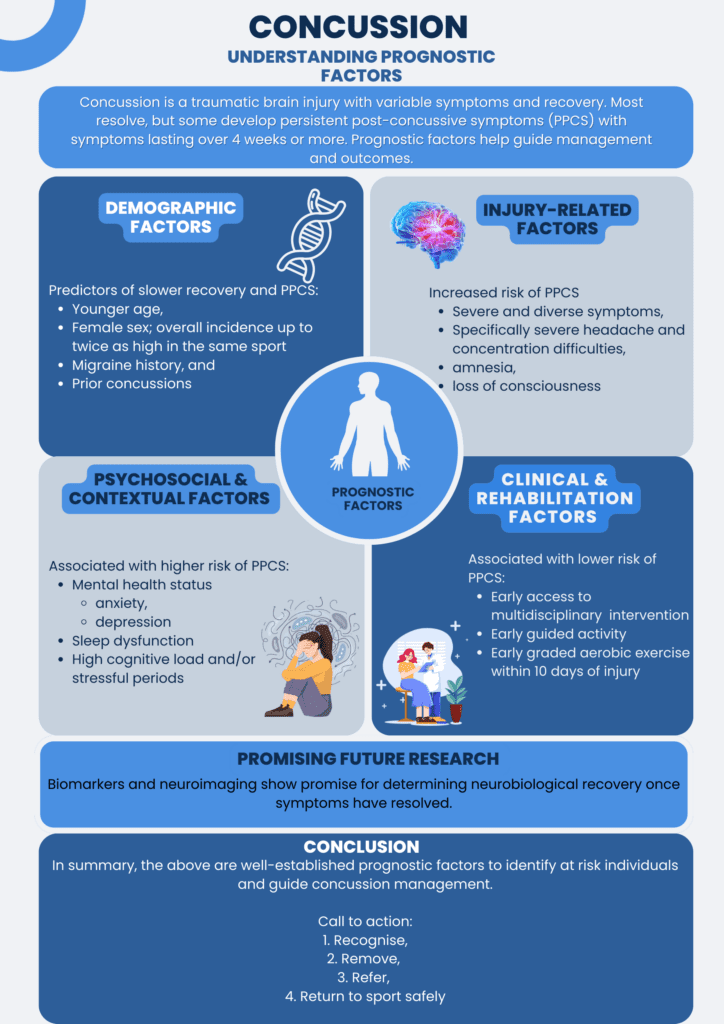
Sport-related concussion is defined as a direct or indirect traumatic brain injury which
results in rapid deceleration of the brain, potential nerve axon injury and inflammation.
The effect is transient brain dysfunction with varying symptoms and varying recovery
time (Patricios et al, 2023). Thankfully, most concussions resolve without complication
post injury (Anderson et al, 2017). Some individuals, however, go on to experience
delayed recovery and “persistent post-concussive symptoms” (PPCS) with symptoms
lasting 4 weeks or more.
Why Prognostic Factors Matter
It is therefore imperative to understand prognostic factors which identify those who are
likely to have a poor outcome and act early. Understanding these factors helps to
stratify risk, guide rehabilitation, and support longer-term decision-making. It also
provides valuable insight into appropriate return-to-play timeframes while assisting in
managing the emotional burden and expectations associated with extended recovery
periods. Importantly, this information is relevant to all stakeholders; including
clinicians, parents, coaches, teachers, and athletes. This ensures a unified and
informed approach to recovery and performance planning.
1. Demographic Factors (non-modifiable)
Younger athletes recover more slowly with adults recovering within 1 to 2 weeks and
children taking up to 4 weeks (Manzanero et al. 2017). It is believed that developing
brains, lax joints and a relatively weaker ratio of cervical muscle to cranium size leads to
less attenuation of forces to the brain (Ferry et al, 2023).
Evidence suggests females may have longer recovery times (McIntosh et al, 2025) and
higher incidence of concussion across a variety of sports. In soccer, the incidence for
men is 3.9% versus women at 5.3%. Similarly in basketball, the incidence for men is
3.2% versus women at 4.7% (Daneshvar et al, 2011).
Past Medical history such as genetic predisposition for migraines or prior concussions
are associated with PPCS and increased complexity in their recovery (McCrory et al,
2017). It was found that athletes who suffered with 1 concussion in the last 2 years had
a 2-fold increase in delayed recovery and a 4-fold increase if 2 or more concussions
occurred.
Given these prognostic factors are non-modifiable, the take home message is to identify
at-risk athletes and consider a more conservative approach.
2. Injury-Related Factors (non-modifiable)
Initial symptom severity and number of different symptoms are associated with
symptom recovery and prognosis. Low symptoms severity and fewer presenting
symptoms are associated with lower risk of developing PPCS. Conversely, high initial
symptom severity and increased number of symptoms are associated with poorer
outcome and risk of developing PPCS. Furthermore, the subset of severe headache,
migraine-like symptoms and concentration difficulties at the time of injury, at 4
weeks and at 12 weeks are strong predictors of prolonged recovery and PPCS (McCrory
et al, 2017).
These are subjectively recorded using a standardised measurement tool such as the
Standardised Concussion Assessment Tool (SCAT 6) or Child SCAT 6 for children 12
years or under (Echemendia et al, 2023).
Finally, concussions sustained with loss of consciousness and amnesia are
associated with a higher risk of developing PPCS with symptoms lasting more than 4
weeks in adults (McIntosh et al, 2025)
3. Psychosocial & Contextual Factors (modifiable)
Mental stressors and mental health status have a significant correlation with severity
and duration of PPCS. Athletes identified with concurrent diagnoses of anxiety,
depression, and sleep disorders are more likely to develop PPCS and delayed return to
school or sport (McIntosh et al, 2025)
It has been shown that students in stressful periods, such as exams, or those in high
cognitively demanding environments have a higher likelihood of developing PPCS after
concussion (Iverson et al 2017).
4. Clinical & Rehabilitation Factors (modifiable)
Early access to intervention is a potent prognostic factor for reducing the delay in
symptom resolution of PPCS (Wade et al, 1998). Individualised intervention with
multidisciplinary care can lead to statistically significant reductions in the Rivermead
Post-concussion Questionnaire with less “social disability” and symptom severity
(Collins et al, 2016). Multidisciplinary care includes vestibular therapy, vision therapy,
psychological support and physical therapies.
Early guided activity compared to absolute rest improves time to recovery. However, a
relative rest period (24-48 hours) should be adhered to once diagnosis and
management strategies have been formalised (McCrory et al, 2017). Similarly, early
graded aerobic exercise, within 10 days of concussion, improves prognosis with
reduced risk of PPCS. (Bogdanowicz et al, 2024)
Conclusion & Key Takeaways
In summary, there are well-established prognostic factors to guide concussion
management.
With easily accessible knowledge and evidence-based protocols, it is imperative that
at-risk individuals are identified early and managed accordingly in a more conservative
manner.
Treatment managing the symptoms of concussion is now well known and easily
accessible. Sports Focus practitioners are trained in managing the symptoms
associated with post-concussive syndrome.
Call to action:
Recognise the signs and symptoms,
Remove the player from the game or training,
Refer them to a medical professional for assessment, and
Return to sport or training only after a complete Graduated Return to Play (GRTP)
protocol
Written by Matthew Grant-Smith
Reference List
Anderson, V., Beauchamp, M. H., Yeates, K. O., Crossley, L., & Ryan, N. (2017). Postconcussion recovery in children and adolescents: A narrative review. Journal of Clinical
and Experimental Neuropsychology, 39(7), 683–697.
https://doi.org/10.1080/13803395.2017.1339102
Bogdanowicz, I., Plante, K., Leddy, J., Master, C., & Haider, M. (2024). Quality of life in
adolescent athletes with sport-related concussion prescribed heart rate-targeted
aerobic exercise within 10 days of injury. Clinical Pediatrics, 64(5), 631–641.
https://doi.org/10.1177/00099228241284345
Collins, M. W., Kontos, A. P., Okonkwo, D. O., Almquist, J., Bailes, J., Barisa, M.,
Bazarian, J., Bloom, O. J., Brody, D. L., Cantu, R., Cardenas, J., Clugston, J., Cohen, R.,
Echemendia, R., Elbin, R. J., Ellenbogen, R., Fonseca, J., Gioia, G., Guskiewicz, K.,
Heyer, R., Hotz, G., Iverson, G. L., Jordan, B., Manley, G., Maroon, J., McAllister, T.,
McCrea, M., Mucha, A., Pieroth, E., Podell, K., Pombo, M., Shetty, T., Sills, A., Solomon,
G., Thomas, D. G., Valovich McLeod, T. C., Yates, T., & Zafonte, R. (2016). Statements of
agreement from the Targeted Evaluation and Active Management (TEAM) approaches to
treating concussion meeting held in Pittsburgh, October 15–16, 2015. Neurosurgery,
79(6), 912–929. https://doi.org/10.1227/NEU.0000000000001447
Daneshvar, D.H., Nowinski, C.J., Mckee, A.C., Cantu, R.C., (2011). The Epidemiology of
Sport-Related Concussion. Clinics in Sports Medicine 30, 1–17.
https://doi.org/10.1016/j.csm.2010.08.006
Echemendia, R. J., Brett, B. L., Broglio, S., Davis, G. A., Giza, C. C., Guskiewicz, K. M.,
Harmon, K. G., Herring, S., Howell, D. R., Master, C. L., Valovich McLeod, T. C., McCrea,
M., Naidu, D., Patricios, J. S., Putukian, M., Walton, S. R., Schneider, K. J., Burma, J. S., &
Bruce, J. M. (2023). Sport concussion assessment tool™-6 (SCAT6). British Journal of
Sports Medicine, 57(11), 622–631. https://doi.org/10.1136/bjsports-2023-107036
Ferry, B., & DeCastro, A. (2023, January 9). Concussion. In StatPearls [Internet].
StatPearls Publishing. Retrieved August 30, 2025, from
https://www.ncbi.nlm.nih.gov/books/NBK537017/
Iverson, G. L., Gardner, A. J., Terry, D. P., Ponsford, J. L., Sills, A. K., Broshek, D. K., &
Solomon, G. S. (2017). Predictors of clinical recovery from concussion: a systematic
review. British journal of sports medicine, 51(12), 941–948.
https://doi.org/10.1136/bjsports-2017-097729
McCrory, P., Meeuwisse, W. H., Dvořák, J., Echemendia, R. J., Engebretsen, L.,
Feddermann-Demont, N., McCrea, M., Makdissi, M., Patricios, J., Schneider, K. J., &
Sills, A. K. (2017). 5th International Conference on Concussion in Sport (Berlin). British
Journal of Sports Medicine, 51(11), 837. https://doi.org/10.1136/bjsports-2017-097699
McIntosh, S. J., Vergeer, M. H., Galarneau, J., Eliason, P. H., & Debert, C. T. (2025).
Factors associated with persisting symptoms after concussion in adults with mild TBI: A
systematic review and meta-analysis. JAMA Network Open, 8(6), e2516619.
https://doi.org/10.1001/jamanetworkopen.2025.16619
Patricios, J.S., Schneider, K.J., Dvorak, J., Ahmed, O.H., Blauwet, C., Cantu, R.C., Davis,
G.A., Echemendia, R.J., Makdissi, M., Mcnamee, M., Broglio, S., Emery, C.A.,
Feddermann-Demont, N., Fuller, G.W., Giza, C.C., Guskiewicz, K.M., Hainline, B.,
Iverson, G.L., Kutcher, J.S., Leddy, J.J., Maddocks, D., Manley, G., Mccrea, M., Purcell,
L.K., Putukian, M., Sato, H., Tuominen, M.P., Turner, M., Yeates, K.O., Herring, S.A.,
Meeuwisse, W., 2023. Consensus statement on concussion in sport: the 6th
International Conference on Concussion in Sport–Amsterdam, October 2022. British
Journal of Sports Medicine 57, 695–711. https://doi.org/10.1136/bjsports-2023-106898
Tabor, J.B., Brett, B.L., Nelson, L., Meier, T., Penner, L.C., Mayer, A.R., Echemendia, R.J.,
Mcallister, T., Meehan, W.P., Patricios, J., Makdissi, M., Bressan, S., Davis, G.A., Premji,
Z., Schneider, K.J., Zetterberg, H., Mccrea, M., (2023). Role of biomarkers and emerging
technologies in defining and assessing neurobiological recovery after sport-related
concussion: a systematic review. British Journal of Sports Medicine 57, 789–797..
https://doi.org/10.1136/bjsports-2022-106680
Wade, D. T., King, N. S., Wenden, F. J., Crawford, S., & Caldwell, F. E. (1998). Routine
follow up after head injury: a second randomised controlled trial. Journal of neurology,
neurosurgery, and psychiatry, 65(2), 177–183. https://doi.org/10.1136/jnnp.65.2.177



